A topline look at a complex topic
Hensin Tsao, MD, PhD, with Cheryl Guttman Krader

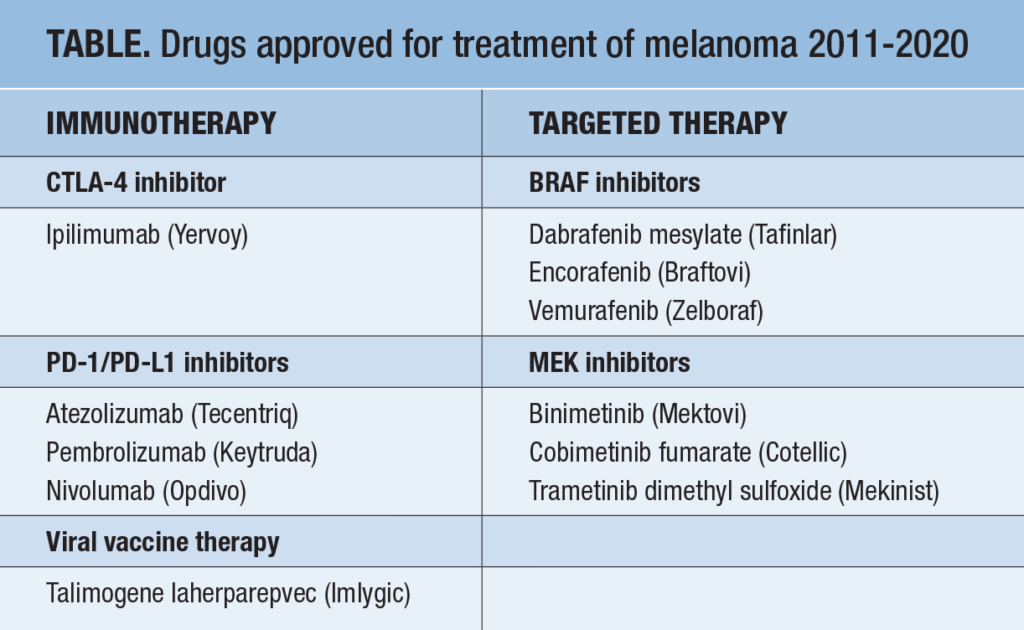
Management for patients with advanced melanoma has changed dramatically over the past decade with an expanding armamentarium of medical therapies approved for the treatment of unresectable disease or as adjuvant therapy following primary tumor resection (Table).
Such a rapid revolution in therapy creates challenges for keeping abreast of the latest management for advanced melanoma, and this complex field continues to evolve as numerous ongoing trials address important questions about treatment sequencing and personalizing treatment selection to optimize outcome.
Dermatologists can look to an American Society of Clinical Oncology (ASCO) practice guideline on systemic therapy for melanoma as a good resource on this topic.1 Considering the number of available treatments as well as the many subtleties and nuances involved in treatment decision-making, care for patients with advanced melanoma requires referral to a medical oncologist.
Looking at the changing landscape of treatment for advanced melanoma, it is amazing to see how far we have come in terms of the number of therapeutic options that have been introduced and their benefit for prolonging survival. Fifteen years ago, the only therapeutic options were cytokine therapy with interleukin-2 or chemotherapy with dacarbazine (DTIC) for stage IV disease, and both of these were of limited efficacy compared to what’s available today. Long-term survival rates for patients with advanced melanoma were just in the 5% to 10% range and there was a general recommendation to encourage patients to enroll in a clinical trial.
When the CTLA-4 inhibitor ipilimumab (Yervoy) became the first systemic therapy approved for melanoma, it was considered an exciting advance. Even though the immune checkpoint inhibitor had significant toxicity, it offered about a 20% likelihood of long-term survival for patients with stage IV disease.2 With today’s treatment regimens, up to 50% of patients achieve long-term survival and some of the options are better tolerated as well.3
ASCO guideline
The 2020 ASCO clinical practice guideline is a 27-page document that provides evidence- and expert-based recommendations across all stages of melanoma, and it is the first of its kind released by the organization. It addresses treatment for both unresectable/metastatic cutaneous melanoma and adjuvant treatment for resected stage II-IV cutaneous melanoma as well as neoadjuvant therapy for resectable cutaneous melanoma and treatment for noncutaneous stage ≥II melanoma.
Patient referral for enrollment in a clinical trial remains the recommendation when considering neoadjuvant therapy for resectable regional or distant metastatic melanoma since the guideline panel felt there was insufficient data to recommend for or against its routine use.
According to the guideline, adjuvant treatment with systemic therapy is standard of care after resection of stage III melanoma. The guideline recommends nivolumab (Opdivo) or pembrolizumab (Keytruda) in the setting of a BRAF wild-type tumor and either of those immune checkpoint inhibitors or combination BRAF/MEK inhibitor therapy with dabrafenib (Tafinlar) plus trametinib (Mekinist) for BRAF-mutant disease.
Eligibility for adjuvant systemic therapy depends on nodal status, especially on findings from sentinel lymph node biopsy.
Some may argue against performing sentinel lymph node biopsy because it does not necessarily improve survival. Nevertheless, the procedure has value because its findings are important for identifying patients as candidates for adjuvant therapy.
For unresectable/metastatic disease, the guideline recommends immunotherapy with ipilimumab plus nivolumab, nivolumab alone, or pembrolizumab alone to treat patients with a BRAF wild-type tumor and any of those choices or combination BRAF/MEK inhibitor therapy with dabrafenib/trametinib, encorafenib (Braftovi)/binimetinib (Mektovi), or vemurafenib (Zelboraf)/cobimetinib (Cotellic) for patients with BRAF-mutated disease. The guideline recommends offering oncolytic virus therapy (talimogene laherparepvec [Imlygic]) as primary therapy for unresectable cutaneous/subcutaneous/nodal lesions when intratumor injection is feasible and the patient is not eligible for or declines systemic therapy.
Approximately one-half of cutaneous melanomas have a BRAF mutation and the others are BRAF wild-type tumors. Whereas immunotherapy would be considered first-line for systemic therapy in the latter setting, medical oncologists vary as to whether they will choose targeted BRAF/MEK inhibitor therapy or immunotherapy first for patients with BRAF-mutated disease.
The ASCO guideline makes no definitive recommendation for choosing between immunotherapy and targeted therapy for these patients and states that the options are listed in no particular order. It is hoped that results from ongoing research will provide guidance on this issue.
Fine-tuning treatment
The good news with the available systemic therapies for melanoma is that about one-half of patients are expected to achieve a durable response. The flip side, however, is that a large number of patients do not achieve such benefit.
An old adage referring to not knowing how the other half lives is very pertinent to patients in the latter situation. Research is needed to develop evidence-based algorithms for care, and there are many studies ongoing.
Investigations underway include studies examining newer approaches for treating patients who do not respond to initial therapy or who lose response over time and also to identify variables, including biomarkers, that might predict response to initial intervention as well as significant toxicity that would lead to treatment discontinuation.
The best ways to use existing and emerging systemic therapies will be defined through accumulating experience and rigorous clinical trials, and that is an area where the medical oncology community excels.
Metastasectomy in the modern era
The effectiveness of systemic therapies for inducing regression of metastases in skin, bone, viscera, and lung raises the question of what role metastasectomy has in patient care. Findings from recent studies show surgery is independently associated with improved overall survival.4-6 The evidence indicates that metastasectomy still has a place. Depending on the patient, it certainly makes sense to attempt to remove readily accessible isolated metastases, treat the patient with adjuvant systemic therapy, and then maintain close follow-up for recurrence and development of new metastatic sites.
The dermatologist’s role
While the primary responsibility for treating patients with advanced melanoma lies in the hands of medical oncologists, the introduction of targeted drugs and immunotherapies for melanoma and other cancers has given rise to oncodermatology as a new dermatology subspecialty that brings dermatologists into the realm of patient care.
The new drugs bring new hope but also new toxicities that spawned a new subspecialty within dermatology focusing on management of treatment-related cutaneous toxicities. BRAF/MEK inhibitors and immune checkpoint inhibitors all cause side effects involving the skin and other body systems that are inflammatory or autoimmune in nature and need to be managed aggressively so that patients can remain on life-prolonging therapy.
It’s rare to see the birth of a new subspecialty, but oncodermatology has emerged to address a true unmet need. Fortunately, many dermatology residents are interested in this field and multidisciplinary teams have been created at Massachusetts General Hospital and other institutions in which dermatologists have a critical role collaborating with oncologists or other specialists in optimizing care for patients with advanced melanoma and other cancers.
REFERENCES
- Seth R, Messersmith H, Kaur V, et al. Systemic therapy for melanoma: ASCO guideline. J Clin Oncol. 2020;38(33):3947-3970.
- Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33(17):1889-1894.
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381(16):1535-1546.
- Elias ML, Behbahani S, Maddukuri S, et al. Prolonged overall survival following metastasectomy in stage IV melanoma. J Eur Acad Dermatol Venereol. 2019;33(9):1719-1725.
- Nelson DW, Fischer TD, Graff-Baker AN, et al. Impact of effective systemic therapy on metastasectomy in stage IV melanoma: a matched-pair analysis. Ann Surg Oncol. 2019;26(13):4610-4618.
- Wollina U, Brzezinski P. The value of metastasectomy in stage IV cutaneous melanoma. Wien Med Wochenschr. 2019;169(13-14):331-338.
DISCLOSURES
Dr. Tsao reports no relevant financial interests.

