
Murad Alam, MD, with Eliza Cabana
“When injecting fillers, what is the risk of vascular occlusion with needles vs cannulas?” It’s the question Murad Alam, MD, and coauthors asked in a retrospective cohort study recently published in JAMA Dermatology.1
“We asked several hundred dermatologists who routinely inject fillers to pull up their records and report how often and exactly in which circumstances they have experienced filler occlusion in the past—when, at which anatomic location, of what level of severity, with which type of filler, and how often,” said Dr. Alam, who is Vice Chair, Chief of Cutaneous and Aesthetic Surgery, and Professor of Dermatology at Feinberg School of Medicine, Northwestern University, Chicago, Illinois. “In addition, we asked them to also let us know how much filler of various types they’ve injected over the preceding 10 years.”

In the context of skin fillers, Dr. Alam says vascular occlusion happens in one of 2 ways: filler either enters a blood vessel through a nick or perforation, or it surrounds and compresses a vessel, thereby preventing blood flow.
Based on data collected, “We were able to get both a numerator and a denominator: How many occlusions divided by how many injections of 1 cc volumes of filler. So, we were able to determine rates of occlusion in different circumstances,” said Dr. Alam. Overall, they found both needles and cannulas to be exceedingly safe. “Even if you use a needle in a relatively ‘higher risk’ area, the likelihood of getting a vascular occlusion is no more than 1 in 6000,” said Dr. Alam. “We found that cannulas can be even less likely to cause occlusions, maybe 1 in 40,000—6 times less likely.” And though it wasn’t part of this study, Dr. Alam points out that when vascular occlusions occur, the vast majority are harmless and resolve without long-term sequelae.
So, needle or cannula?
Although the study shows the risk for vascular occlusion is significantly lower when injecting with cannulas, needles are very safe and still have a place in the injectable filler armamentarium. “We’re certainly not saying ‘don’t use a needle’ or ‘needles are dangerous,’” said Dr. Alam. “What we are saying is, in some instances— when it’s appropriate given the anatomic site, the kind of filler, the patient requirements—it may be helpful to consider a cannula. But it’s a complex decision made on a variety of factors, and only the patient and the physician collaboratively can decide if it’s appropriate or not.”
Although the study provides no insight into the exact set of circumstances in which to choose a cannula rather than a needle, certain factors could make a needle the better choice. But, said Dr. Alam, there are so many that it’s difficult to generalize.
“No one has studied the dozens of possible permutations of factors to see which ones are better or worse, so I don’t want to pretend to have any special knowledge on this. There are certain situations—for instance, when I’m injecting very superficially, or when I want to know exactly where the filler is going—when it is sometimes easier to be very precise with a needle,” he said. Another question the researchers did not address was the risk of blindness specifically. Instead, they measured severity by grade: grade 1 (no sequelae), grade 2 (scar), and grade 3 (ocular injury or blindness). “We didn’t really focus on the most severe complication of vascular occlusion, which is blindness, because this wasn’t the primary aim of our study, and because we were worried that if we asked for much greater detail about filler-associated vision problems, people might not be so forthcoming with their data,” explained Dr. Alam.
A learning curve
According to the study, there is a slight learning curve for less-experienced injectors. Those with more than 5 years of experience had 70.7% lower odds of having an occlusion than less-experienced injectors, with a 1% decrease in odds for every additional injection/week. While it was more likely for occlusions to take place in the nasolabial fold and lip areas, the most severe occlusions took place in the glabella.
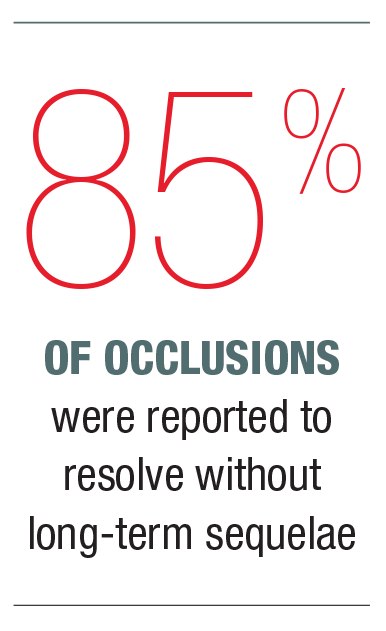
Nevertheless, Dr. Alam pointed out that the learning curve for dermatologist injectors is relatively short and serious occlusions happen very infrequently—85% were reported to resolve without long-term sequelae. “We found a couple of reassuring things. First of all, it didn’t require an enormous amount of experience for board-certified dermatologists to perform filler injections very proficiently. But as with most things that require some hand-eye coordination, there is a learning curve. We know there are some areas where, regardless of the instrument used, there is a greater risk of vascular occlusion. These include the glabella, around the nose, [and] some other watershed areas where there are lot of vessels in a small space.” Thus, while it may be prudent for the less-experienced dermatologist injector to avoid the higher anatomic risk zones for filler injection, this does not change the fundamental truth that minimally invasive filler injections are highly effective and exceedingly safe.
Vascular occlusion happens
Redness, blanching, and pain are all associated with occlusion, but these tell-tale signs are all also often part of the normal injection process, which can complicate identifying an occlusion. “Even if you don’t have a vascular occlusion, a little bit of redness, a little bit of a blanch [from lidocaine], and a little bit of pain do occur when filler is injected,” said Dr. Alam. “It can be extremely difficult to differentiate at the time of injection if the redness, the whiteness, and the pain are normal, or if they’re elevated enough to increase suspicion for vascular occlusion.”
Another factor is the fact that people have different pain thresholds. “So, it’s very important to make sure your receptionists, your nurses, and your medical assistants know that, after filler injection, if someone calls the next morning and they’re having discomfort, they shouldn’t just be reassured. If the degree of discomfort seems excessive, you want to advise them that their coming in and being seen would be a good idea.”
Study limitations
Dr. Alam acknowledged that the actual rates of vascular occlusion could be slightly different than those reported due to memory and/or documentation inaccuracies. “This is based on retrospective data,” said Dr. Alam. “So, we did ask people to look through their medical records. In some cases, respondents may have supplemented their medical records with their memories of past events, and we do believe that a vascular occlusion—even a relatively benign one—is something that people generally remember well.”
Overall, Dr. Alam said that the researchers were not surprised to find that cannulas have a lower occlusion rate. “But it’s nice to know there’s some data behind that now,” he said. That being said, Dr. Alam noted that their study shows the safety of filler injections only when performed by board-certified dermatologists. He added, “Our study does not say anything about the safety of filler injections performed by less-well-trained injectors, non-dermatologists, or non-physicians.”
REFERENCES
- Alam M, Kakar R, Dover JS, et al. Rates of vascular occlusion associated with using needles vs cannulas for filler injection. JAMA Dermatol. 2021 Feb 1;157(2):174-180. doi: 10.1001/jamadermatol.2020.5102.
DISCLOSURES
Dr. Alam reports no relevant financial interests.

