With Kelly M. Cordoro, MD, and Carmel Aghdasi, BA
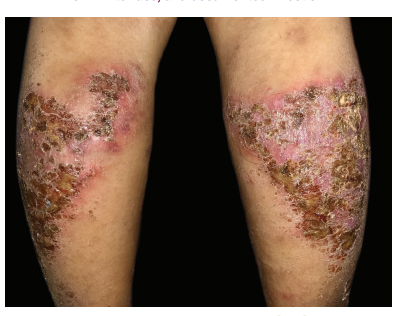
Data presented at the Society for Pediatric Dermatology: 2021 Annual Meeting is helping to advance knowledge on epidemiology, clinical features, comorbidities, and evolving treatment patterns for pediatric psoriasis.
In a retrospective cohort study of 754 psoriasis patients ages 0 to18 years seen at the University of California, San Francisco (UCSF) from 1997 to 2021, researchers found that systemic, biologic, and phototherapy usage varies by age group and treatment decade.
“There has been a substantial increase in the use of systemic and biologic therapies over time, which is an important step in bridging the treatment gap for moderate-to-severe pediatric psoriasis patients,” noted Carmel Aghdasi, BA, one of the study authors. “Specifically, between 2001 and 2011, conventional systemics and biologics were used primarily in adolescents. Between 2012 and 2021, this trend changes—we saw conventional systemic use increase in infancy and childhood and decrease in adolescents, while biologic use increased in all age groups, most substantially in children aged 3 to 12 years. Over this same time frame, phototherapy use decreased in adolescents, was stable in childhood, and increased in infants.”
“We found that risk factors for moderate-to-severe psoriasis include increasing age, morphology (guttate, plaque + guttate, and pustular/erythrodermic), non-white race, and documented infection,” said Kelly Cordoro, MD, senior author of the study. “Notably, obesity was not associated with psoriasis severity in this cohort. Concurrent infection was strongly associated with increased psoriasis severity and should be sought and managed. Further analysis of this data set aims to shed light on the finding that race influences severity.”
Dr. Cordoro noted these findings are important given the rise in and availability of systemic treatment options.
“The treatment data over time represent an objective measure of the shifting treatment landscape for children with psoriasis. The current era, with more pediatric patients included in therapeutic trials and thus more objective safety and efficacy data, features the approval of several systemic therapeutic options for pediatric psoriasis. This should prompt greater comfort with systemic therapies for children among dermatologists and improved access to medications. Ideally, this will result in adequate treatment of children suffering with moderate to severe psoriasis who historically have been undertreated.”
The study authors say more research is needed.

“Further analysis of our data set is ongoing,” noted Aghdasi. “One area we hope to shed light on is the finding that race influences severity; further investigation of the role of concurrent infection on disease course and severity is also needed.”
“Outside of our data, there is much left to do, such as assess equity and access to care among pediatric patients, clarify the relevance and prognostic value of comorbidities such as obesity in childhood in terms of later onset of cardiovascular morbidity, and define the natural history of various types of psoriasis and the influence of treatment on long-term physical and mental health and other comorbidities,” said Dr. Cordoro.
By Nayda Rondon
DISCLOSURES:
Data analysis was performed in collaboration with Dr. Barbara Grimes from UCSF Clinical and Translational Science Institute (CTSI Grant #UL1 TR000004). UCSF Yearlong Inquiry Program supported this program.

