Diagnosing and Treating the Burning, Itch, Pain of Sensitive Skin
With Enzo Berardesca, MD
Dr. Enzo Berardesca discusses overcoming the challenges of sensitive skin, from diagnosis to treatment and management.
“… sensitive skin [is] a syndrome defined by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations,” according to a definition by the special interest group on sensitive skin of the International Forum for the Study of Itch.1
Sensitive skin can be challenging for the practicing dermatologist to diagnose because patients do not typically present with cutaneous signs of the syndrome.
“Dermatologists are used to seeing skin disease. And [when] these patients describe suffering from sensitive skin, you don’t see anything,” said Enzo Berardesca, MD, Research Professor in Dermatology at the University of Miami Miller School of Medicine, author of Sensitive Skin Syndrome,2 and member of the special interest group on sensitive skin of the International Forum for the Study of Itch, which wrote the “Pathophysiology and management of sensitive skin: position paper,” published February 2020 in the Journal of The European Academy of Dermatology and Venereology.
“Sometimes there is a little bit of redness. Sometimes the redness lasts a few seconds or minutes and then disappears,” Dr. Berardesca said. “So, sensitive skin is a subjective condition. The dermatologist should trust what the patient says and claims to suffer.”
While skin barrier abnormalities are frequently associated with sensitive skin, there is not proven direct relationships between the two, Dr. Berardesca and coauthors report in their position statement.
“Now studies show that sensitive skin is also a problem in the nerve endings—in particular, in the small fiber nerve endings, which are the thinner endings going into the skin. There is a hyperactivity of these fibers, and, in patients with sensitive skin, the fiber gets excited. There is a release of cytokines, which … cause inflammation and the stinging, burning, itching, and so on. This is called the neurogenic theory,” he said.
Making the Diagnosis
Dermatologists who suspect sensitive skin syndrome can ask patients to fill out a standardized questionnaire (such as the Sensitive Scale3), which scores skin sensitivity.
“There also is a test, called the Lactic Acid Stinging Test, which is done by applying a cotton ball moistened with a solution of lactic acid of 10% or 15%, on the nasolabial fold. After applying the lactic acid … you have to wait a few minutes and usually if the patient suffers from sensitive skin, the patient will feel something—stinging, burning, itching, or something like that,” Dr. Berardesca said.
“Triggers for sensitive skin can be everything, but, I would say, mainly chemicals.”
Possible triggers include cosmetic products. Soaps with surfactants can easily irritate sensitive skin.
“Even water can be a trigger. Other factors are reported to be environmental, including sun exposure and sudden changes in temperature. Wind and cold can be a trigger. Some foods, like alcohol or spicy food, can increase vasodilatation in the vessels of the face …, which can be associated with stinging, burning, and itching,” Dr. Berardesca said.
Treating, Managing Sensitive Skin
“The dermatologist should do an accurate analysis of the patient and try to avoid these triggering factors,” he said.
Patients need to be aware of what is good and not good for their skin.
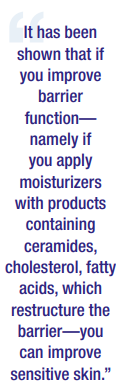
“Products that are designed to improve or treat sensitive skin are designed to improve barrier function. It has been shown that if you improve barrier function—namely if you apply moisturizers with products containing ceramides, cholesterol, fatty acids, which restructure the barrier—you can improve sensitive skin.”
“There are new products coming out which can modulate the neurogenic inflammation and the overactivity of these nerve endings…,” he said.
In the position paper, the authors suggest pruritogens, which target dermal and epidermal nerves, act via different receptors and ion channels such as TRPA1 and TRPV1.
“… one study demonstrated the successful use of a novel topical TRPV1 agonist in 30 patients with sensitive skin,” according to the statement.
However, without a clear understanding of the pathogenesis of sensitive skin, there is no “gold standard” treatment. The position paper authors recommend a holistic, personalized approach that considers possible biomedical, neural, and psychosocial factors; trigger avoidance,; damaged skin barrier restoration; photoprotection; and anti-inflammatory agents, as well as psychological support.
By Lisette Hilton
References
- Misery L, Weisshaar E, Brenaut E, et al. Pathophysiology and management of sensitive skin: position paper from the special interest group on sensitive skin of the International Forum for the Study of Itch (IFSI). J Eur Acad Dermatol Venereol. 2020;34(2):222-229. doi:10.1111/jdv.16000.
- Berardesca, E., Maibach, H.L., & Fluhr, J.W. (Eds.). (2006). Sensitive Skin Syndrome (1st ed.). CRC Press. https://doi.org/10.3109/9781420004601
- Misery L, Jean-Decoster C, Mery S, Georgescu V, Sibaud V. A new ten-item questionnaire for assessing sensitive skin: the Sensitive Scale-10. Acta Derm Venereol. 2014;94(6):635-639. doi:10.2340/00015555-1870
Disclosure: Dr. Berardesca is a consultant of Bioderma, Clarins, Nestle Skin Health, and Pierre Fabre.