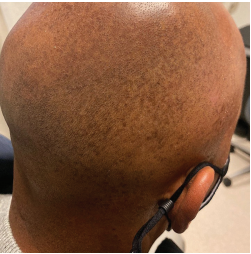
Diffuse, Splotchy Scalp Hyperpigmentation with Variable Scaling Erythema
By Ted Rosen, MD, FAAD
CASE HISTORY
A 60-year-old African American male presented for evaluation of a rash limited to his scalp, which had been present for approximately five years.
The patient complained that the eruption was periodically itchy and scaly, noting that he avoided wearing dark shirts and sweaters because of the heavy “dandruff.” The patient noted that this typically worsened in the winter and improved somewhat in the spring and summer. He vehemently denied rubbing his head, and essentially never wore a hat or cap.
The patient’s other illnesses included sleep apnea and low-grade chronic back pain. He had no known allergies and only took aspirin, as needed, for back pain. He denied any other prescription or over-the-counter medications or supplements.
He was a retired schoolteacher, with an unremarkable social history. Family history was positive for ischemic heart disease, but the patient himself had no cardiac complaints.
Physical examination revealed diffuse splotchy hyperpigmentation of the scalp, extending onto retroauricular skin. (See photo) The scalp itself appeared somewhat oily. There were small patches of fine scale present.
A potassium hydroxide preparation of the scales was negative. Examination of the scalp with a Woods lamp failed to show coral-red fluorescence. The patient’s vital signs were normal, and a recent set of biochemical and hematological studies done as part of a routine physical examination were entirely normal.
Although a small punch biopsy was strongly suggested, the patient adamantly declined. Instead, he preferred a therapeutic trial based upon our “best guess.”
What is your diagnosis?
DISCUSSION
The diagnosis is seborrheic melanosis, a rare variant of seborrheic dermatitis. This entity consists of localized darkening of the seborrheic areas, with variable scaling and erythema admixed.
It is seen in those with Fitzpatrick skin types IV and above, having been noted in African Americans, Asians, Hispanics, and those of Indian ancestry.1,2
Seborrheic melanosis may be itchy or entirely asymptomatic. It characteristically worsens during cold, dry months and improves to a varying degree during humid months. This pattern was seen in our patient. Another interesting feature is sparing of several areas where classic seborrhea occurs–the eyebrows and eyelids.3
Those who have written about this entity do not believe it to be merely an expression of post-inflammatory hyperpigmentation to seborrhea because there are usually some signs of active inflammation, and the typical interventions solely aimed at pigment removal fail. Instead, therapy consists of application of anti-inflammatory and/or anti-fungal agents known to be effective in the treatment of active seborrhea (topical calcineurin inhibitors, mild-moderate potency topical steroids and 2% ketoconazole cream).2
This individual was treated with ketoconazole 2% cream and hydrocortisone 1% cream, each once daily. He was also instructed to start wearing a hat when outdoors to reduce ultraviolet light stimulation of melanogenesis. A teledermatology visit some five months later showed that the melanosis, scale, and itch had all resolved.
References:
- Verma SB, Vasani RJ, Chandrashekar L, Thomas M. Seborrheic melanosis: An entity worthy of mention in dermatological literature. Indian J Dermatol Venereol Leprol. 2017;83(3):285-289. doi:10.4103/0378-6323.203248.
- Vashisht KR, Garg S. Seborrheic Melanosis: A Unique Under-recognized Entity in Ethnic Skin. J Clin Aesthet Dermatol. 2022;15(1):15-16.
- Arshdeep, Sonthalia S, Kaliyadan F, et al. Seborrheic melanosis and dermoscopy: Lumping better than splitting. Indian J Dermatol Venereol Leprol. 2018;84(5):585-587. doi:10.4103/ijdvl.IJDVL_175_18.