Continued Explosion of Sexually Transmitted Disease
by Ted Rosen, MD
Data from 2019 collected by the Centers for Disease Control and Prevention (CDC) indicated that, for the sixth consecutive year, the incidence of sexually transmitted disease (STD) continued to increase.
STD data for any given year is typically available in September or October of the following year. However, 2020 data collection, collation and reporting were delayed due to the justifiable CDC preoccupation with the COVID-19 pandemic.
The 2020 data was eagerly anticipated because nobody knew exactly what to expect. Would shelter/work at home recommendations and requirements, social distancing rules, mask-wearing mandates, bar closures, increased depression and anxiety, and the virtual death of large group gatherings going to lead to a decrease in STDs?1 Or, would fewer overall visits for health care, closure or severe restrictions of STD clinics nationwide, more available idle time due to layoffs or curtailed work schedules, and worldwide condom and antibiotic shortages lead to a continuing increase in STDs?1
The wait is finally over, and the picture is bleak.
Of course, the statistics need to be interpreted with caution. The COVID-19 pandemic led to major disruptions in STD-specific services. Only about 8% of all STD clinics operated normally; many others were periodically or completely closed due to lack of personal protective equipment or due to a configuration and/or size which was not conducive to social distancing.2,3 Other STD clinics limited or entirely eliminated preventative testing and prophylactic treatment, only caring for those who presented with acute signs and symptoms suggestive of STDs.2,3 There was also a shortage of trained STD health care intervention personnel, as many were reassigned to COVID-related tasks.
Thus, if anything, incomplete STD case report collection may have led to a significant underestimate of the 2020 U.S. STD burden.
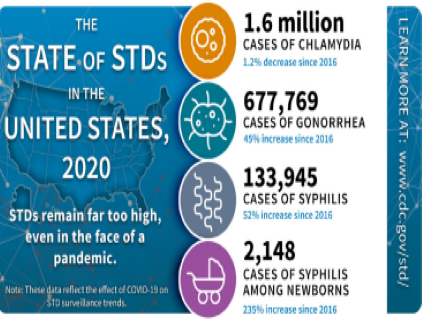
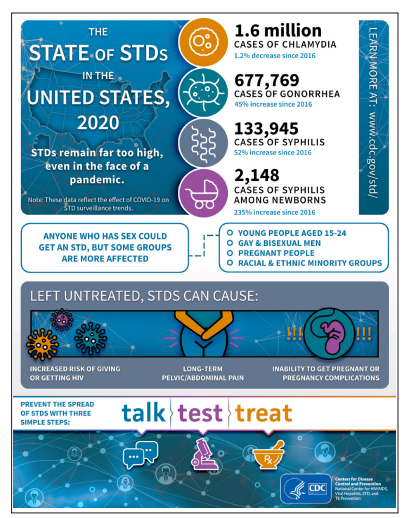
Nonetheless, the CDC press release of April 12, 2022, was a grim reminder that STDs have not disappeared in the middle of the pandemic.4 While cases of chlamydia decreased slightly, the other reportable STDs increased compared to 2019. For example, reported cases of gonorrhea increased by at least 10%, going from 616,392 to 677,769; reported cases of syphilis (all stages) increased at least 3.2%, going from 129,813 to 133,945 – with the largest gain coming in primary and secondary syphilis of 7%.4
Most tragically, reported 2020 cases of congenital syphilis rose nearly 15%, going from 1870 to 2148.4 The number of 2020 cases of congenital syphilis represents a remarkable increase of 235% compared to 2016.
Epidemiologic trends noted in previous years continued. Fifty-three percent of all reported STD cases were diagnosed in adolescents and young adults, aged 15 to 24.4,5
Some racial and ethnic groups remain harder hit than non-Hispanic Whites. Thirty-two percent of all reported cases of chlamydia, gonorrhea, and primary and secondary syphilis (the most contagious form) occurred in non-Hispanic Black individuals, even though that group only comprises about 12% of the U.S. population.5
Men who have sex with men (gay, bisexual) are also disproportionally impacted by STDs, particularly syphilis and all forms of uncomplicated gonorrhea.5 These disparities likely reflect a number of factors, such as lack of access to regular medical care or difficulty in obtaining sexual health care, some element of discrimination, stigmatization of those with known STDs, and differences in the individuals’ sexual network (ie. partners often drawn from a social pool characterized by high STD prevalence).
It wasn’t that long ago when the CDC was talking about syphilis eradication in America! Sadly, this goal seems farther away than ever.
The CDC press release and the accompanying full report6 reinforce the need for dermatologists to refresh their skills regarding the diagnosis and treatment of STDs that predominantly manifest on the cutaneous surface.
By the way, preliminary statistics for 2021 don’t look any better. Even as delayed case reports are still being submitted, there is already a 34% increase among women and a 9% increase among men of primary and secondary syphilis, and a 6% increase in congenital syphilis!7
Historically, dermatologists were highly involved in the STD world. Now is not the time to ignore these disorders, as they are resurgent. Now is not the time to abrogate STI diagnosis and therapy to other specialties that do not have the training or skill sets to accurately diagnose STDs, and offer up treatment in a timely fashion.
Now is the time to recommit to being the expert, the community resource, regarding these most important diseases.
References:
- Wiggins CJ, Rosen T. Sexually Transmitted Diseases in the COVID-19 Era. Skinmed. 2020;18(4):210-212. Published 2020 Aug 1.
- Wright SS, Kreisel KM, Hitt JC, et al. Impact of the COVID-19 Pandemic on Centers for Disease Control and Prevention-Funded Sexually Transmitted Disease Programs. Sex Transm Dis. 2022;49(4):e61-e63. doi:10.1097/OLQ.0000000000001566.
- CDC. Impact of COVID-19 on STDs. Sexually Transmitted Disease Surveillance 2020. Accessible at: www.cdc.gov/std/statistics/2020/impact.htm. Accessed June 15, 2022.
- CDC. New data suggest STDs continued to increase during first year of the COVID-19 pandemic. 2022; April 12. Press Release. Accessible at: 2020 STD Surveillance Report Press Release | Newsroom | CDC. Accessed June 15, 2022.
- CDC. Disparities in STDs. Sexually Transmitted Disease Surveillance 2020. Accessible at: www.cdc.gov/std/statistics/2020/overview.htm#Disparities. Accessed June 15, 2022.
- CDC. New Data Show that STDs Remain Far Too High. Sexually Transmitted Disease Surveillance 2020. Accessible at: www.cdc.gov/std/statistics/2020/default.htm. Accessed June 15, 2022.