A rare subset of T cells known as Vd1-gd T cells can help predict which melanoma patients may benefit most from immunotherapy, according to research in Nature Cancer.
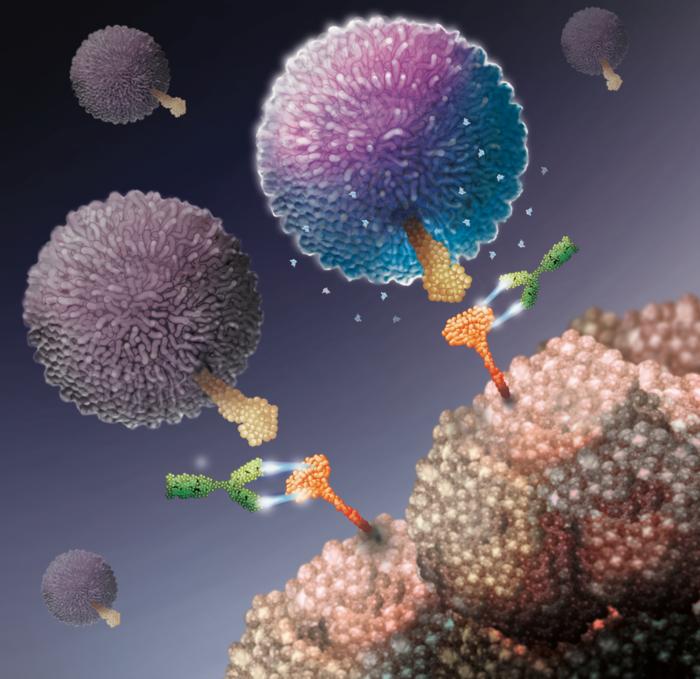
Previous research has shown that immune checkpoint inhibitors (ICIs) can ‘reactivate’ T cells formerly suppressed by cancer cells. The T cells can then kill cancer cells by recognizing cancer cell mutations that are not present in healthy cells.
“The number of cancer mutations can sometimes help doctors identify the patients most likely to benefit from ICI therapy but curiously, some cancers with very few mutations can still respond very well,” explains study author Dr. Yin Wu, a Wellcome Trust Clinician Scientist at King’s College London and Honorary Consultant Medical Oncologist at Guy’s Hospital in London.
The research team reasoned that these successes must be due to other immune cells that can see cancer cells even in the absence of lots of mutations.
Enter Vd1-gd T cells.
These T cells can recognize and kill cancer cells without needing them to have mutations for identification. These cells can be found inside tumors where they also have a specific type of immune checkpoint protein, PD-1.
The researchers analyzed clinical trial data from 127 patients with melanoma who were treated with ICIs that targeted the “PD-1” immune checkpoint and found that the presence of Vd1-gd T cells was highly predictive of positive responses to ICI therapy, particularly in cancers with few mutations.
The team then used a new technique to isolate and grow these cells from human tissues and showed for the first time that the Vd1-gd T cells can be reactivated by ICI therapies currently used in the National Health Service to treat patients with advanced skin cancer.
Personalized Medicine in Action
“The study findings may help doctors decide which patients are most likely to benefit from current immunotherapies,” says study author Dr Shraddha Kamdar, a Research Fellow at King’s College London. “These therapies are both costly and importantly can cause severe and life-long side effects, so it is important to be able to predict when they will actually work.”
The team also found evidence that the Vd1-gd T cells could be more resistant to suppression from cancer cells compared with more common T cells, meaning that therapies using Vd1-gd T cells could work for longer periods.
Study author Daniel Davies, a PhD student, adds, “Our study highlights the importance of understanding the contributions of lesser-studied immune cell types in efforts to improve the effectiveness of immunotherapies.”
These findings may help doctors decide which cancer patients would benefit most from certain immunotherapy treatments. The ability to predict whether a patient will have a high chance of responding will save medical service providers from ordering costly treatments that may not work and help prevent patients from undergoing potentially toxic treatments that won’t help their cancer.
Study author Adrian Hayday, Professor of Immunobiology at King’s College London and Principal Group Leader at the Francis Crick Institute, says, “The study’s results are striking, and strongly support ongoing efforts to directly infuse Vd1-gd T cells into patients with cancer, an approach pioneered at King’s College London and the Francis Crick Institute.”