By Ted Rosen, MD, FAAD and Usman Asad, MD
Case History
A 59-year-old African American female presented for evaluation of pruritic lesions involving the right neck and left hip. Lesions had been present and solely expanding over the preceding two to three years.
Past medical history was significant for pulmonary sarcoidosis for four years. Although once symptomatic, the lung sarcoidosis was clinically quiescent at the time of presentation. The patient denied both shortness of breath at rest and dyspnea on exertion. Recent biochemical panel was entirely within normal limits.
Physical examination revealed several atrophic, white-brown colored scar-like plaques on the left hip and a solitary similarly appearing plaque on the right medial, inferior neck. There was some hyperpigmentation at the periphery of the plaques.
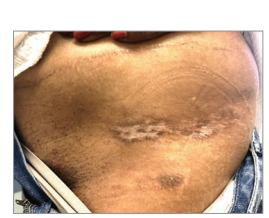
The patient denied lesions elsewhere and specifically denied genital lesions. She had been successfully treated for a symptomatic vulvovaginal yeast infection in the recent past. A biopsy was performed.
What do you think the diagnosis turned out to be?
Discussion
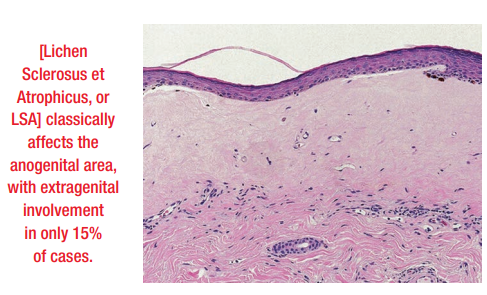
Biopsy revealed an orthohyperkeratotic stratum corneum with epidermal atrophy and patchy vacuolar interface change. There was a significant homogenized/edematous papillary dermis and mild lichenoid dermal lymphocytic infiltrate.
The diagnosis is extragenital lichen sclerosus (or Lichen Sclerosus et Atrophicus/LSA). LSA classically affects the anogenital area, with extragenital involvement in only 15% of cases. Women are affected more commonly than men. There is a bimodal occurrence: pre-pubertal girls and then 40- to 50-year-old women. In adult men, LSA typically affects the glans penis and may result in phimosis. LSA may be associated with a variety of autoimmune disorders. Sarcoid is not a classical association, however.
In addition to atrophy and hypopigmentation, hemorrhage and fissuring may also be seen clinically in any LSA lesion. Extragenital LSA is usually asymptomatic but can itch or develop a feeling of dryness. Most common sites of extragenital disease include the upper trunk/neck, proximal upper extremities, flexor wrists, and areas of pressure (shoulder, hip). Oral lesions are quite uncommon, but lips, gingiva, palate, tongue, or buccal mucosa may demonstrate irregular, white or hypopigmented plaques.
First line treatment for LSA, regardless of the site or sites involved, consists of daily application of an ultrapotent steroid. Randomized, blinded studies have shown clobetasol to be superior to a topical calcineurin inhibitor. Topical calcineurin inhibitors remain the second choice for therapy. Persistent, refractory lesions may be treated with phototherapy (UVA1 or NB-UVB) or systemic immunosuppressives (steroids, methotrexate). Risk of evolution into squamous cell carcinoma in genital LSA is about 5%. A comparable, reliable statistic for extragenital disease does not exist.

