By John Jesitus | Reviewed by Todd Schlesinger, MD
The efficacy of newer medications including inhibitors of hedgehog (HH) and programmed death-1 (PD-1) signaling carries the caveat that prescribers must monitor for multi-systemic adverse events (AEs), which may be severe. Additional considerations with both drug categories include resistance and, for HH inhibitors (HHIs), potential drug interactions.
Checkpoint inhibition
“The difference with PD-1 immune checkpoint inhibitors versus prior medications is that the side effects we see are immune-mediated,” said Todd Schlesinger, MD. “Once you activate the immune system to fight the tumor, the immune system can attack other parts of the body as well. It’s important to remember that the adverse events from these new immunotherapy medications can affect almost every organ system.” Dr. Schlesinger is Director of the Dermatology and Laser Center of Charleston and the Clinical Research Center of the Carolinas, both in Charleston, South Carolina.
Previously, treatment for advanced cutaneous squamous cell carcinoma (CSCC) that was not a candidate for surgery or radiation, including locally advanced (laCSCC) and metastatic tumors (mCSCC), involved cytotoxic and/or platinum-based chemotherapy. Epidermal growth factor receptor inhibitors such as cetuximab signaled the next evolutionary phase.
The above treatments seek to kill or inhibit growth of the tumor itself. However, Dr. Schlesinger added, these therapies were never FDA-approved for CSCC and provided response rates of around 20%, with significant adverse events (AEs).
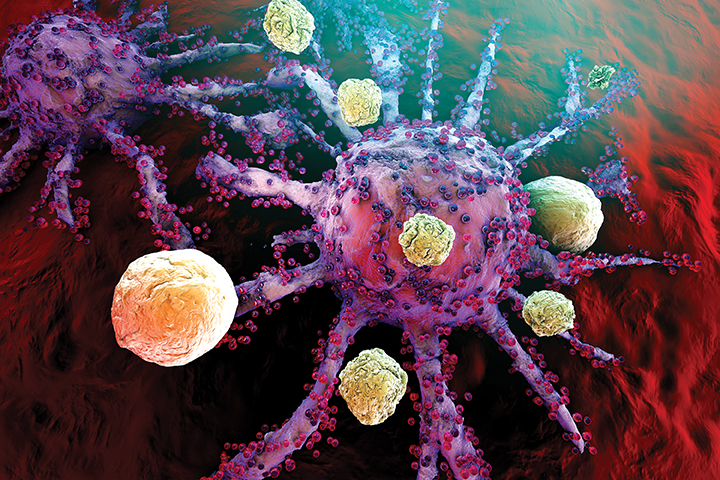
Eventually, he said, the discovery of tumor-cell and T-cell receptors proved that CSCC tumors can “cloak” themselves. “They figure out how to protect themselves from the immune system by presenting receptors on their surface that tell the immune system the tumors are part of the body’s own tissue.” As a result, circulating T cells that are supposed to attack the tumors essentially ignore them.
Unlike prior therapies, the checkpoint inhibitors pembrolizumab (Keytruda, Merck) and cemiplimab (Libtayo, Regeneron and Sanofi Genzyme) can activate cytotoxic immune cells such as CD8 and other cells to infiltrate and destroy CSCCs.
“That has shifted the paradigm from attacking the tumor directly toward helping the body’s own immune system fight the tumor,” said Dr. Schlesinger.
Cemiplimab earned FDA approval in 2018 for patients with mCSCC or laCSCC who are not candidates for curative surgery or radiation. Pembrolizumab earned approval in 2020 for recurrent CSCC or mCSCC not curable by surgery or radiation. In pivotal trials, these drugs achieved overall response rates (ORRs) of 46.1% and 34.3%, respectively.1,2 With cemiplimab, average time to response was 2.1 months. Duration of response (DOR) lasted at least 6 months in 91% of patients; 99.5% of patients experienced AEs. With pembrolizumab, the 2-month progression-free survival rate was 32.4%, and 66.7% of patients experienced treatment-related AEs.
The systems most commonly impacted by checkpoint-inhibitor AEs include the lungs, gastrointestinal tract, and skin, said Dr. Schlesinger. Fortunately, he added, most of these AEs are mild-to-moderate and easily treatable with medications such as corticosteroids. 1,2,3
Nevertheless, Dr. Schlesinger said, identifying serious AEs early is crucial, as they require at least temporary (grade 3) or permanent (grade 4) drug discontinuation. In a safety analysis of cemiplimab in basal cell carcinoma (BCC), 17% of patients experienced AEs leading to discontinuation.3
“Physicians who are [prescribing] these medications should be attuned to symptoms that that they might otherwise not pay much attention to, such as cough, fatigue, rash, or diarrhea.” Additionally, Dr. Schlesinger recommended full laboratory evaluations, including thyroid function and glucose metabolism.
Hedgehog inhibition
FDA-approved in 2012, vismodegib (Erivedge, Genentech) offers ORRs in metastatic BCC (mBCC) and locally advanced BCC (laBCC) of 48.5% and 60.3%, respectively, at 39 months, with DOR lasting 4.8 and 26.2 months, respectively.4 Sonidegib (Odomzo, Sun Pharma) earned approval in 2015 for locally advanced recurrent BCC or BCC not amenable to surgery or radiation. In pivotal research, sonidegib demonstrated 6-month ORRs of 43% in laBCC and 15% in mBCC.5 Median DOR was 26.1 months in laBCC, but not evaluable in mBCC.
HHI-related AEs may stem from the presence of the HH pathway in non-tumoral tissues such as taste buds, said Dr. Schlesinger. The most common treatment-emergent AEs for the approved 200-mg sonidegib dose included muscle spasms, alopecia, and dysgeusia, which affected 38% to 49% of patients. Grade 3 and 4 AEs affected 27% and 4% of patients in this cohort, respectively. A subsequent 1215-patient global safety study (STEVIE) showed similar rates of the most common AEs; 31% of patients experienced AEs leading to treatment discontinuation.6
“Patients were getting side effects from these medications,” said Dr. Schlesinger, “so the treatment was being interrupted.” Fortunately, he said that with HHIs, tumor response tends to appear before AEs, which provides assurance that these drugs are working.
The STEVIE study moreover showed that most vismodegib side effects decline significantly over time. For example, incidence of muscle spasms dropped from 98% to 4.9% during the trial. “The muscle spasms and hair loss that patients initially experience in the first 12 months of therapy tend to settle down after one year,” Dr. Schlesinger said.
The MIKIE trial showed that cycles of 12 or 24 weeks, with an 8-week break between cycles, provided similar efficacy to that seen in pivotal vismodegib studies, with fewer side effects.7 “This is a way that you can keep these patients on therapy longer, by using an interrupted dosing schedule,” said Dr. Schlesinger.
To temporarily ameliorate HHI side effects, physicians may offer supportive treatments such as minoxidil 5% BID for alopecia and nutritional consults for dysgeusia and/or weight loss.8 For muscle spasms, options include amlodipine 10 mg daily8 or levocarnitine. The latter reduced muscle spasm frequency by 48% in a 4-week, double-blinded, randomized placebo-controlled pilot trial.9
The potential for drug interactions with sonidegib also warrants consideration. “Patients taking medications that can affect the hepatic metabolism pathway via cytochrome P450 may need a dose adjustment for sonidegib,”10 said Dr. Schlesinger. That is not the case, he added, for patients taking sonidegib who experience mild-to-moderate renal impairment or mild hepatic impairment.
Resistance to HHI therapy has driven additional research into adjuvant and co-treatment options. Mutations in the transmembrane protein Smoothened (Smo), HHIs’ primary target, account for up to half of advanced BCCs resistant to both vismodegib and sonidegib.11,12 Researchers have hypothesized that by targeting alternate stages of the HH pathway, drugs such as arsenic trioxide, itraconazole, all-trans retinoic acid, and nicotinamide may bypass or forestall HHI resistance.13
“Polychemotherapy could play a role in patients with basal cell carcinoma,” says Dr. Schlesinger. Because arsenic trioxide and itraconazole increase QT intervals, he added, these drugs require caution in patients with cardiac disorders and in those taking other drugs that prolong the QT interval.
Regarding CSCC, the FDA recently granted fast-track status to AST-008 (cavrotolimod, Exicure) in combination with anti-PD-1 or anti-programmed death-ligand 1 (PD-L1) therapy for laCSCC or mCSCC refractory to prior anti-PD-1/PD-L1 blockade; and in combination with PD-1 blockade for locally advanced or metastatic Merkel cell carcinoma refractory to prior anti-PD-1 therapy.
REFERENCES
1. Rischin D, Khushalani NI, Schmults CD, et al. Phase 2 study of cemiplimab in patients with advanced cutaneous squamous cell carcinoma (CSCC): longer follow-up. Poster 367. American Society of Clinical Oncology (ASCO) 2020 Virtual Scientific Meeting. May 29-31, 2020.
2. Grob JJ, Gonzalez R, Basset-Seguin N, et al. Pembrolizumab monotherapy for recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase ii trial (KEYNOTE-629). J Clin Oncol. 2020;38(25):2916-2925.
3. Stratigos AJ, Sekulic A, Peris K, et al. LBA47—Primary analysis of phase II results for cemiplimab in patients (pts) with locally advanced basal cell carcinoma (laBCC) who progress on or are intolerant to hedgehog inhibitors (HHIs). Ann Oncol. 2020;31(suppl_4):S1142-S1215.
4. Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366(23):2171-2179.
5. Migden MR, Guminski A, Gutzmer R, et al. Treatment with two different doses of sonidegib in patients with locally advanced or metastatic basal cell carcinoma (BOLT): a multicentre, randomised, double-blind phase 2 trial. Lancet Oncol. 2015;16(6):716-728.
6. Basset-Séguin N, Hauschild A, Kunstfeld R, et al. Vismodegib in patients with advanced basal cell carcinoma: Primary analysis of STEVIE, an international, open-label trial. Eur J Cancer. 2017;86:334-348.
7. Dréno B, Kunstfeld R, Hauschild A, et al. Two intermittent vismodegib dosing regimens in patients with multiple basal-cell carcinomas (MIKIE): a randomised, regimen-controlled, double-blind, phase 2 trial. Lancet Oncol. 2017;18(3):404-412.
8. Lacouture ME, Dréno B, Ascierto PA, et al. Characterization and management of hedgehog pathway inhibitor-related adverse events in patients with advanced basal cell carcinoma. Oncologist. 2016;21(10):1218-1229.
9. Cannon JGD, Tran DC, Li S, Chang AS. Levocarnitine for vismodegib-associated muscle spasms: a pilot randomized, double-blind, placebo-controlled, investigator-initiated trial. J Eur Acad Dermatol Venereol. 2018;32:e298–e299.
10. Villani A, Fabbrocini G, Costa C, Scalvenzi M. Sonidegib: safety and efficacy in treatment of advanced basal cell carcinoma. Dermatol Ther (Heidelb). 2020;10(3):401-412.
11. Pricl S, Cortelazzi B, Dal Col V, et al. Smoothened (SMO) receptor mutations dictate resistance to vismodegib in basal cell carcinoma. Mol Oncol. 2015;9(2):389-397.
12 Atwood SX, Sarin KY, Whitson RJ, et al. Smoothened variants explain the majority of drug resistance in basal cell carcinoma. Cancer Cell. 2015;27(3):342-353.
13. Cosio T, Di Prete M, Campione E. Arsenic trioxide, itraconazole, all-trans retinoic acid and nicotinamide: a proof of concept for combined treatments with hedgehog inhibitors in advanced basal cell carcinoma. Biomedicines. 2020;8(6):156.
DISCLOSURES
Dr. Schlesinger has been a consultant and researcher for Genentech (vismodegib), Regeneron and Sanofi Genzyme (cemiplimab), and Sun Pharma (sonidegib).