Sheila Fallon Friedlander, MD, with Bob Kronemyer
For difficult pediatric warts, there are viable treatments other than cryotherapy and salicylic acid.
“Several newer breakthroughs are combination therapies which offer new options, such as combining cryotherapy with immunization or combining different intralesional (IL) treatments like tuberculin purified protein derivative (PPD) and Candida,” said Sheila Friedlander, MD, a staff dermatologist at Scripps Clinic in San Diego and a Professor Emeritus in Dermatology at the University of California San Diego School of Medicine. “You can also use the human papillomavirus (HPV) vaccine.”

In her presentation on warts at Maui Derm Connect 2021 titled “Maui Derm Peds Style,” Dr. Friedlander cited a study that was published last year in the Journal of the American Academy of Dermatology (JAAD) that alternated IL agents for warts.1 “I have been discussing IL Candida for years now,” she said. “I use it all the time in kids who have warts. The beauty of IL Candida is that you can treat 1 or 2 lesions, often achieving a systemic immunologic effect and all the warts resolving.”
Dr. Friedlander nearly always pretreats the sites with cryotherapy, “which appears to provide a bit of anesthesia to the site,” she said.
The study divided patients into 4 groups, all of whom were injected with 0.1 mL into the largest wart every 2 weeks for up to 6 treatment sessions as needed: IL PPD; IL Candida 1/1000; alternating PPD and Candida; or saline.
Among the 143 patients who completed the study, complete clearance occurred in 61% of patients administered PPD; 36.8% of patients given Candida; 70.6% of patients with the alternating therapy (P < 0.0001); and 8.6% of patients with saline.
“I think these outcomes are exciting for recalcitrant disease,” Dr. Friedlander said. “Why not alternate PPD with Candida?”
A second study from last year’s JAAD compared IL to intramuscular (IM) bivalent HPV vaccine for recalcitrant warts.2
For the study, 22 patients were given an IM injection at 0, 1, and 6 months. Another 22 patients were given an IL injection into their largest wart every 2 weeks until clear, or 6 injections total.
Overall, 82% of patients in the IL group attained complete clearance compared to 63% in the IM group.
A 9-valent HPV vaccine is available as well. “So instead of being limited to 2 HPV subtypes, we now have an additional 7: 16, 18, 31, 33, 45, 52, and 48,” she said. “Might this vaccine do a better job with warts? I think this is definitely the way to go and hopefully we will have more studies looking at the use of a 9-valent HPV vaccine.”
When Dr. Friedlander sees a patient in the office with bad warts, the first question she asks is if the patient has had an HPV vaccine. “If the patient has not, and is aged 7, 8 or 9, I will encourage the patient to get the vaccine,” she said. “ I also want to make sure there is no sign of immunosuppression.”
Occasionally, children may suffer from conditions such as dedicator of cytokinesis 8 (DOCK8) deficiency, which may present with severe warts or molluscum. “Ask if the patient has had recurrent pneumonia or otitis,” Dr. Friedlander said. “When in doubt, refer to an immunologist.”
What are the guidelines for HPV vaccination? “We know that the risk of exposure to HPV increases with age,” she said. “We also know that the vaccine is not as effective after your patient has been infected.”
The Advisory Committee on Immunization Practices and the American Cancer Society recommend that everyone between the ages of 9 and 12 be vaccinated. A catch-up vaccination can be administered up to age 26. “Thus, if you have a patient who comes in who is older, you want that person to get vaccinated,” Dr. Friedlander said. “But the vaccine is not necessarily beneficial for older people.”
Still, the vaccination is recommended for people between the ages of 27 and 45 who have multiple sexual partners or are at high risk for HPV for other reasons.
There was a time when Dr. Friedlander was very excited about oral zinc sulfate to treat warts. “I tried it on a number of patients, but many reacted with stomach aches,” she said. “I also cannot recall a patient who got better.”
A double-blind study published in 2018 in the International Journal of Women’s Dermatology compared cryotherapy plus oral zinc sulfate to cryotherapy plus placebo for warts.3 “The bottom line is that the zinc did not make much of a difference,” said Dr. Friedlander.
“Although controversial, some believe that if a patient actually has a low serum zinc level, zinc therapy for warts may be more efficacious. There are no large controlled studies to support this, but occasionally practitioners will check zinc levels and use zinc if the level is below normal,” she added.
WartPEEL cream (NuCara Pharmacy) is a non-FDA-approved product that “people are very excited about,” Dr. Friedlander said. “Despite the lack of much literature, many patients are now using it and coming back to the office saying it is really helpful.”
The cream is a combination of 17% salicylic acid and 2% 5-fluorouracil in an adhesive vehicle that leads to sustained release. “It is not regular duct tape, but a plastic tape that very slowly releases this agent,” Dr. Friedlander said. Patients apply the cream at night, then remove it in the morning and clean the wart.
One cream kit costs $80 and is generally not covered by insurance.
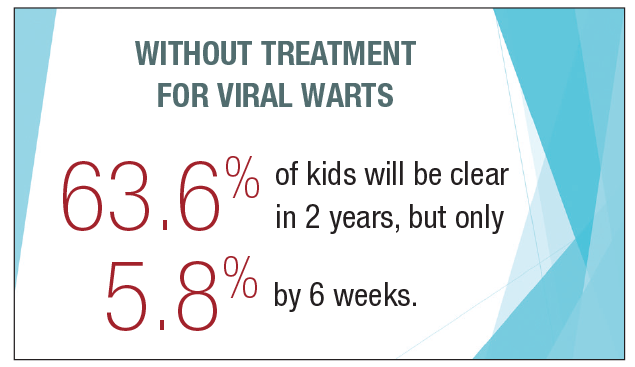
A 2020 literature review of viral warts in children in Dermatologic Therapy reveals that without treatment, 63.6% of kids will be clear in 2 years, but only 5.8% by 6 weeks.4 The review also found that cryotherapy in the canister is equivalent to cotton wool (Q-tip) application, “which is against my own experience,” Dr. Friedlander said. “But the authors say if you apply liquid cotton wool to the tip of a cotton swab and place it on the wart, it will be as effective as a cryotherapy spray gun.”
In addition, the literature review concluded that immunotherapy topical clearance rates were 88% for diphenylcyclopropenone (DPCP), 60% for bacillus Calmette-Guerin (BGC) and 71% to 87% for Candida.
“The authors also said it is not unreasonable to follow non-palmoplantar warts; however, palmoplantar warts are unlikely to go away on their own,” Dr. Friedlander said.
Disclosures
Dr. Friedlander reports no relevant financial interests.
References
1. Nofal A, Yehia E, Khater E, Bessar H. Alternating intralesional purified protein derivative and Candida antigen versus either agent alone in the treatment of multiple common warts. J Am Acad Dermatol. 2020 Jul;83(1):208-210. doi:10.1016/j.jaad.2020.01.054
2. Nofal A, Marei A, Ibrahim ASM, et al. Intralesional versus intramuscular bivalent human papillomavirus vaccine in the treatment of recalcitrant common warts. J Am Acad Dermatol. 2020 Jan;82(1):94-100. doi:10.1016/j.jaad.2019.07.070
3. Mahmoudi H, Ghodsi SZ, Tavakolpour S, Daneshpazhooh M. Cryotherapy plus oral zinc sulfate versus cryotherapy plus placebo to treat common warts: a double blind, randomized, placebo-controlled trial. Int. J Womens Dermatol. 2018 Jun;4(2): 87–90. doi:10.1016/j.ijwd.2017.09.004
4. Soenjovo KR, Chua BWB, Wee LWY, et al. Treatment of cutaneous viral warts in children: a review. Dermatol Ther. 2020;33:e14034.

