By Robert Kronmeyer |Reviewed by Moise Levy, MD
Treating ichthyosis and other disorders of cornification in children and adolescents with either topical or systemic retinoids, or both, is not only generally safe, but also can be highly effective in reducing scaling and improving function and appearance, according to consensus recommendations published in November 2020 in the journal Pediatric Dermatology.

“There is lack of a uniform approach to the use of retinoids in childhood cases of ichthyosis,” said co-author Moise Levy, MD, a Professor of Pediatrics and Medicine at Dell Medical School, The University of Texas at Austin. “However, these recommendations should not come as a surprise to dermatologists, even though up until now guidance for systemic retinoids has not existed.”
The guidance was crafted by a variety of experts in dermatology, ophthalmology, reproductive health, and retinoids, as well as input from the Foundation for Ichthyosis and Related Skin Types (FIRST).
To increase the efficacy of retinoids in this patient population, the dermatologist must “first and foremost engage the patient or family as to what they are seeking in a very basic level from therapy,” Dr. Levy said.
Retinoids are known to have an impact on skin turnover. “Because retinoids influence cell development, retinoids have been considered for years as potentially useful in this group of conditions,” Dr. Levy said. “What you see as a provider with retinoids is a patient with reduced scaling and thickness of the skin. Such effects are hopefully achieved from use of a topical or a systemic retinoid.”
Topical vs systemic
The decision whether to use topical or systemic retinoids depends mostly on the extent of disease. For instance, is therapy specifically for eyelid closure or specifically to lessen thickening of skin on palms and/or soles? Or to improve these sites and also the skin on the torso and extremities?
“If you are trying to treat a very focal area, a topical is clearly the way to go and preferable to a systemic,” Dr. Levy said. “But for larger areas of the body impacted by the condition, a systemic retinoid should be considered for use.”
For topical therapy, Dr. Levy tends to prescribe tazarotene, despite patient insurance challenges. Retinoid alternatives are tretinoin and adapalene, which fall within the same class as tazarotene.
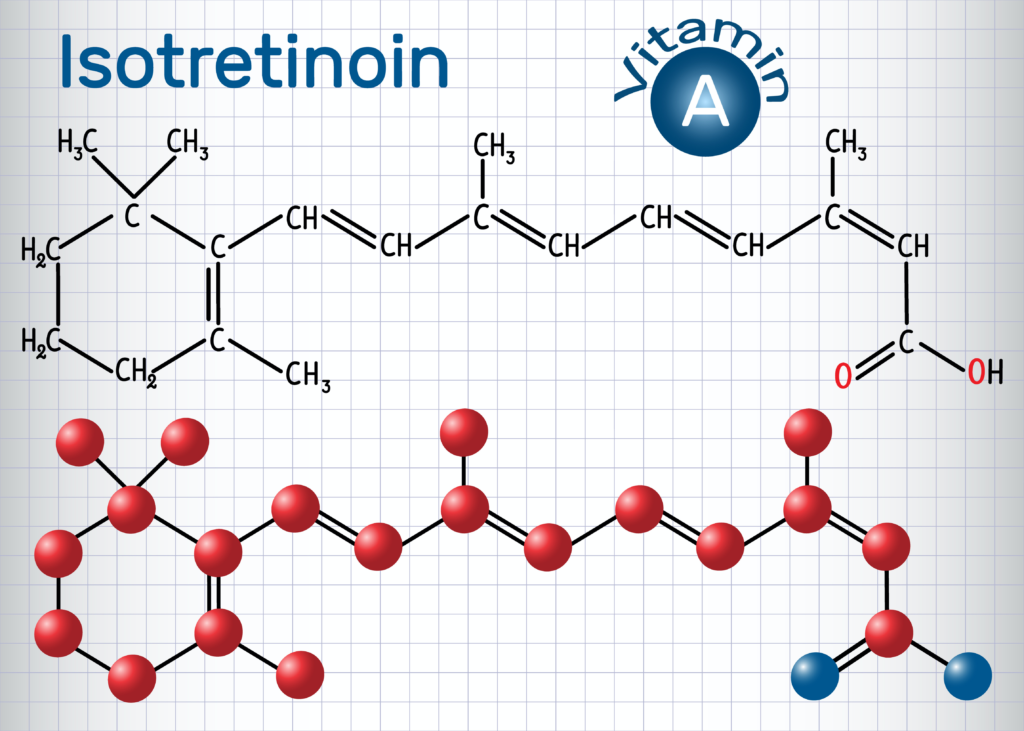
For systemic therapy, most dermatologists have used either acitretin or isotretinoin, the latter specifically approved for acne; however, acitretin remains in the body for up to 3 years, according to Dr. Levy. “Therefore, acitretin becomes a concern when discussing toxicities, should they develop, or their impact on unborn children,” he said. “Instead, we might try isotretinoin, particularly in kids. Compared to acitretin, though, isotretinoin has a much shorter duration of action. For that reason, many physicians favor starting with isotretinoin, if not continuing with the drug, because if any issue develops you can stop the drug and the medication is cleared far more rapidly than with acitretin.”
The iPLEDGE program serves as the Risk Evaluation and Mitigation program for isotretinoin, with which all patients and prescribers of isotretinoin must comply. “Adherence to the guidelines, however, can be quite cumbersome, because iPLEDGE was not developed with ichthyosis in mind, which potentially requires years of therapy,” Dr. Levy said.
For systemic retinoid dosing, the lowest dose possible to achieve the desired clinical outcome is recommended.
However, duration varies between topical and systemic. “For topicals, there is no specific duration that you need to consider, assuming the patient does not have any side effects from the therapy, such as local irritation,” Dr. Levy said. “But for systemic treatment, there are isolated cases of bone toxicity or reproductive concerns among individuals capable of pregnancy and of appropriate age. These considerations might limit duration and timing of therapy.”
Side effects and safety
Because all these medications are vitamin A derivatives, systemic retinoids affect bone, and there are isolated reports of closure of the growth plates, particularly in children, and calcification on the soft tissues (tendons and ligaments) around bones. “Retinoids may also cause bony overgrowth along the spine, which can lead to pain,” Dr. Levy said. “All these bone issues need to be considered at the onset of therapy. There may also be a family history of such problems.”
Furthermore, systemic retinoids may cause dry eye, and to a lesser degree, corneal opacities.
In addition, both isotretinoin and acitretin can occasionally cause elevations in serum lipids or adversely affect liver function. “Nonetheless, we monitor lipid levels and the liver before treatment and at intervals during therapy,” Dr. Levy said. “With lipid elevation, there is potential concern about cardiovascular impact from prolonged and elevated levels in the blood.”
Psychiatric effects of systemic retinoid therapy also continue to be an area of discussion, particularly for isotretinoin. “These psychiatric changes, though, occur less frequently in the cohort of patients receiving those drugs than occur in the general population,” Dr. Levy said. “But we still ask patients about their psychiatric well-being while on these medications. If there is any noted change, we will engage a behaviorist to help.”
Patients who could become pregnant and are sexually active should use 2 forms of contraception, including 1 highly effective form, while on any systemic retinoid therapy, either short- or long-term. “There is great risk to an unborn fetus for a multitude of birth defects,” Dr. Levy said. “Thus protection from pregnancy is absolutely indicated.”
The guidelines underscore that providers must be aware of what is known and unknown about the safety and efficacy of long‐term retinoid use. “Risks should be discussed candidly with patients and their families through shared decision-making and recognize that long‐term safety data are lacking,” Dr. Levy said.
The intention of the guidelines is not to be the final word. “Rather, these recommendations are a platform upon which more data will be delivered,” Dr. Levy said.
Commentary
Monitoring and modifications needed
None of the recommendations for retinoids in treating ichthyosis and other disorders of cornification in children and adolescents should come as a surprise to dermatologists, according to Amy Paller, MD, a Professor and Chair of Dermatology at Northwestern University in Chicago. “However, there may be monitoring suggestions that are new to clinicians or unmet needs that may resonate,” she said.
For patients who require oral retinoids for a long duration, “we prefer to use isotretinoin because it is safer than acitretin, especially among young women,” Dr. Paller said. “But the iPLEDGE program still needs to be in place for any use of isotretinoin. Any patient who uses the drug in the long term as a safer retinoid is burdened by the program, including pregnancy testing every month and connecting with the office monthly to receive their next dose. This is a huge obstacle, especially for prescribing [for longer than] 6 months.”
Dr. Paller hopes the continuing unmet need of dispensing isotretinoin can be resolved through modifications in the iPLEDGE program. “Our adolescent girls and young adult women have a lifelong disorder that demands responsibility, including pregnancy avoidance while on a retinoid,” she said. “Some monitoring is needed, but less often than monthly would be appreciated.”
Paller noted that the alternative retinoid, acitretin, has no associated iPLEDGE-like program, but is retained in fat and thus requires a 2- to 3-year period off medication (vs 1 month with isotretinoin) when considering pregnancy.
In addition, not all disorders of cornification with scaling respond to retinoids. “In fact, some do worse; for example, Netherton syndrome should probably not be considered for retinoids,” Dr. Paller said. In contrast, patients with lamellar ichthyosis can greatly benefit from retinoids.
The guidelines for following patients long-term, including ocular and bone monitoring, are valuable. Techniques for administering a retinoid capsule to a child who cannot swallow are also contained in the guidelines.
Dr. Paller added, “Most of these patients carry huge burdens, including the highly visible nature of the disorder, reduced ability to sweat, and the itch and pain associated with their ichthyosis. For many patients, retinoids—whether topical or systemic—can drastically alter their disease course, but only if they are used.”
These guidelines for the pediatric population will give dermatologists more confidence in prescribing retinoids, both topically and systemically, for children with disorders of cornification, according to Dr. Paller. “We want clinicians to understand the potential toxicity of retinoids, but risk is minimized by monitoring,” she said.
Dr. Paller advocates standardizing monitoring of patients so that uniform information can be collected for safety.