By John Jesitus
Identifying the development of aggressive squamous cell carcinoma (SCC) after en bloc excision of hidradenitis suppurativa (HS) requires more careful monitoring and a high index of suspicion, experts tell The Dermatology Digest.
Over the past decade, said Afsaneh Alavi, MD, new biologic therapies for HS have shed light on this orphan disease, resulting in more papers and meeting sessions on HS. Dr. Alavi is a dermatologist at the Mayo Clinic in Rochester, Minnesota.
The biologic-driven narrative highlights improvements in patients’ health and quality of life, said Neal Bhatia, MD. “But there’s little discussion of other hidden issues like squamous cell existing in patients with hidradenitis suppurativa.” He is Director of Clinical Dermatology at Therapeutics Clinical Research in San Diego, California.
In a case series published in Dermatologic Surgery in April 2019, researchers led by John J. Kohorst, MD, searched Mayo Clinic Rochester records from 1976 through 2013 and found 12 cases in which SCC arose after HS resection.1 Nine patients were male; the cancers affected the gluteal (n = 8), perianal (n = 6), perineal (n = 4), and/or vaginal (n = 1) areas. At a mean follow-up of 4.3 years after wide excision, SCC recurred in 7 patients—all of whom ultimately died.
SCC arising in the setting of HS is very uncommon, said lead author John J. Kohorst, MD, a Mohs surgeon at the Mayo Clinic Health System in La Crosse, Wisconsin.
“But when it does occur, the mortality is very high. It’s something we’re always on the lookout for because when it does happen, it can be deadly.”
Often, he added, certain subtypes of SCC can be very aggressive. “And in the setting of a chronic inflammatory disease like hidradenitis, all of us as clinicians need to be thinking about the possibility of squamous cell carcinoma because it can go undetected and evolve into a high-grade skin cancer.”
The presence of numerous inflammatory papules and nodules in the area increases the difficulty of distinguishing whether a painful inflammatory papule is secondary to HS or may represent an SCC, said Dr. Kohorst. “So these squamous cell carcinomas can go undetected, grow, and then spread prior to being recognized, biopsied, and treated.”
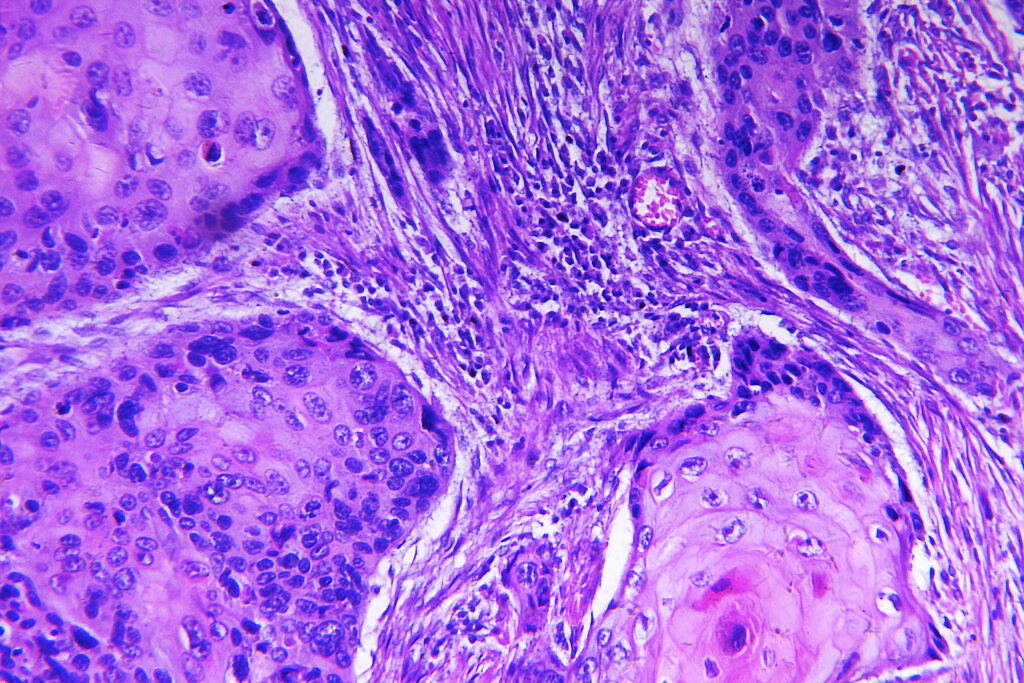
Dr. Bhatia said, “Compared to basal cell carcinoma, with squamous cell carcinoma you get a lot of lateral spread under the microscope. It’s a much more aggressive tumor once it hits the dermis.” [SO2] The poorly differentiated subtype found in many of Dr. Kohorst et al.’s patients can be even more difficult to capture with a clean margin, Dr. Bhatia added.
The predominance of male patients in the series slightly surprised Dr. Kohorst. In a 2016 review of surgical outcomes in 590 patients, Dr. Kohorst and his colleagues found that 60% of patients were male.2 “So it’s not entirely shocking that those who develop squamous cell carcinoma were mostly males,” he said. “Why the percentage was that high, I can’t say.”
Dr. Alavi added that even though the Dr. Kohorst’s studies and a 2015 review on which she was senior author3 showed a predominance of cases in men, she has also seen cases of HS with SCC in females.
It is also unclear why SCC so often strikes the perianal/perineal area. In the 2016 report, the most common HS site was perianal/perineal (49.8%), followed by the axilla (21%). Dr. Kohorst said, “It’s possible that SCC could arise in any area affected by hidradenitis. Common things being common, the 2019 study supports our surgical data showing that areas commonly affected by severe hidradenitis are most commonly the groin and the axilla, with a slight predominance toward male patients.”
Although experts previously believed that human papilloma virus (HPV) contributed to SCC development in HS, said Dr. Alavi, Dr. Kohorst et al.’s 12-patient series showed no evidence of HPV. “This shows that a chronic, long-standing ulcer is enough to cause these aggressive cancers,” Dr. Alavi said. This study also showed that even at one of the best treatment centers, many patients experience postsurgical HS recurrence, added Dr. Alavi.
When viewed by surgery type, Dr. Alavi’s 2015 review revealed HS recurrence rates for wide excision, local incision, and de-roofing of 12%, 22%, and 27%, respectively.3 A single-center study involving 75 patients (most with Hurley stage III disease) showed an overall postsurgical HS recurrence rate of 35%.4 The only risk factor significantly linked with recurrence was 1-stage surgical closure.
Early detection
Because HS cannot be prevented or cured, early detection and management of both HS and subsequent SCC are paramount. However, diagnostic difficulties abound.
Dr. Alavi said, “It’s not easy because we see patients in the dermatology clinic who have lots of draining lesions and usually are obese or large patients.” Adequately illuminating these patients’ perianal, perineal, and genital areas is challenging, she said. “That’s why many of these cancers are diagnosed when they are too advanced to do anything.” In Dr. Kohorst’s 2019 case series, mean HS duration before SCC diagnosis was 28.5 years.
Dr. Bhatia added that patients with HS are often first diagnosed as having acne, cysts, and abscesses. “Given the area—the axillary distribution or the perineum—the index of suspicion for hidradenitis should be pretty high,” he said. Instead of just getting antibiotics from their primary care doctors, said Dr. Bhatia, these patients should be evaluated by dermatologists quickly, and probably prescribed biologics more quickly than in the past.
Ongoing follow-up is equally critical. “If someone has had long-standing, difficult-to-medically-control hidradenitis,” said Dr. Kohorst, “it’s important for us as clinicians to be seeing them regularly. More frequent follow-up is a good thing for these patients.” He leaves the follow-up interval to the discretion of individual dermatologists. Dr. Bhatia suggests a frequency of at least every 6 months.
Patients should examine themselves often, added Drs. Alavi and Bhatia. However, noted Dr. Alavi, the perianal area is difficult for patients to see, and they cannot differentiate between HS ulceration and SCC formation. “I encourage patients to seek advice and ask for an exam if they have any concern.”
Dr. Bhatia said, “The American Academy of Dermatology does a good job with the SPOT Skin Cancer [public awareness] program. I would probably tell these patients, ‘Your risk might not be as high as someone with more sun damage, but the types of cancer you could get would be more aggressive. That should raise your concern for looking more often.’”
HS detected in early stages can be managed medically, said Dr. Alavi. With antibiotics (first-line) and biologics (second-line), she said, some patients require anti-androgens. But eventually, she said, most patients—she estimates 70%, based on current patient patterns—require surgery combined with medical therapy.
To shrink tumors before excision, Dr. Bhatia said that dermatologists now can use cemiplimab (Libtayo, Regeneron and Sanofi). “Many dermatologists aren’t familiar with cemiplimab’s use. It is the newest therapy we have for this type of squamous cell carcinoma—invasive and advanced.”
Interdisciplinary teamwork
To manage these complex cases, Drs. Kohorst, Alavi, and Bhatia recommend interdisciplinary care. “As dermatologists,” said Dr. Kohorst, “we can do a lot. But there are other specialties that have expertise in this area.”
In his 2016 case review, HS resections were performed by general surgeons (51.4%), plastic surgeons (35.8%), dermatologists (10.3%), and other specialties (2.5%), including gynecologic surgeons. “And still, many of these patients, depending on their access to dermatologists, are going to be seeing their primary care physicians a lot. Having them on board is also very important in managing these patients, who are very difficult to manage and treat,” Dr. Kohorst said.
At the University of Toronto, where Dr. Alavi formerly worked, surgery, dermatology, and nursing make up the core of the multidisciplinary care program. Providers in these specialties seek assistance from other disciplines including psychiatry, gastroenterology, and nutrition as needed. “Surgery and dermatology should work together hand-in-hand to manage patients with HS from the beginning,” said Dr. Alavi.
Dr. Bhatia added, “The dermatologists should be the quarterback for these patients. They should be directing the traffic. And then the rest of the team—the oncologists and radiation oncologists—would pass the patient back.”
Dr. Alavi said she hopes that using more multidisciplinary care for patients with HS will reduce the number of long-standing ulcers that dermatologists see. Over time, she added, diagnosing and treating HS earlier will result in less tissue damage, better outcomes, and fewer surgeries.
To refine care algorithms for these patients, Dr. Kohorst recommends additional research. To date, most studies have been small case reports and series.
“With chronic wounds like hidradenitis suppurativa,” said Dr. Alavi, “we are hoping that clinicians are cognizant of the presence of malignancy that may be under diagnosed because it’s in a difficult location—the perianal area. A good exam with proper light helps early detection, and we need to have a low threshold for biopsy when the patient has a lesion in this area.”